Imagine looking in the mirror and not knowing who is looking back at you, or suddenly realizing you no longer know how to cook eggs. It’s a frightening image, but one that is all too real for the more than 55 million people worldwide currently suffering from Alzheimer’s disease or other forms of dementia.
It is a disease that not only impacts the patients, but also those who love them.
“I have been working in research for aging and dementia my entire life, and it still did not prepare me for when my grandmother was diagnosed with dementia,” said Dr. Karienn Souza, a research assistant professor in Texas A&M University’s College of Medicine. “She was incredibly smart, funny and kind. She spoke four languages, and the disease took that away from us. And not only was that devastating, but there was nothing we could do. There was no treatment to cure it. There’s no way to prevent it. There’s really no way to truly slow it down.”
But there may be hope on the horizon through a new, innovative treatment being investigated by Dr. Ashok Shetty, a University Distinguished Professor of cell biology and genetics in Texas A&M’s College of Medicine, and associate director of the Texas A&M Institute for Regenerative Medicine.
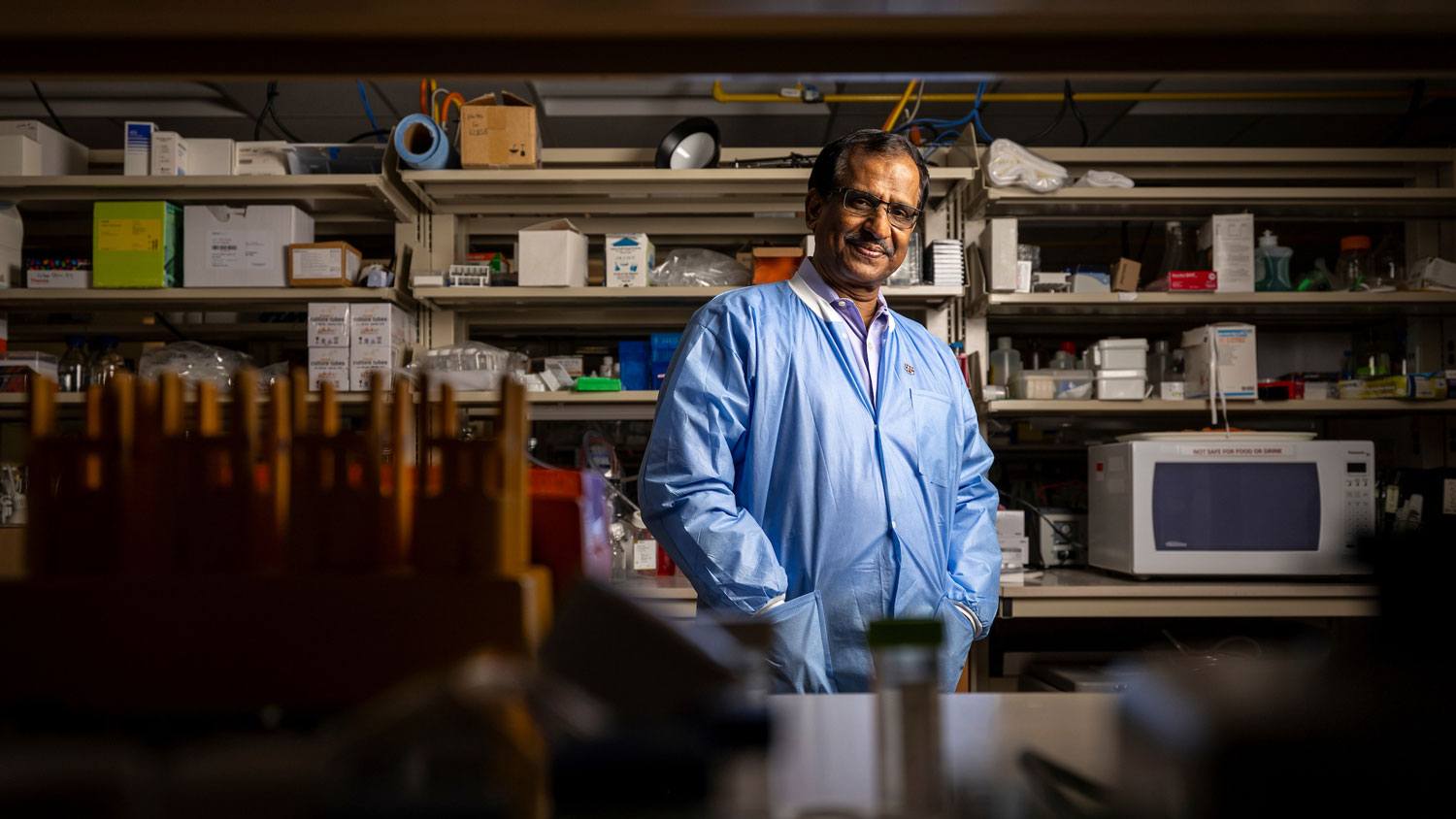
Interested from a young age in learning about how the brain works, Dr. Ashok Shetty is committed to finding an effective and accessible treatment for Alzheimer’s disease.
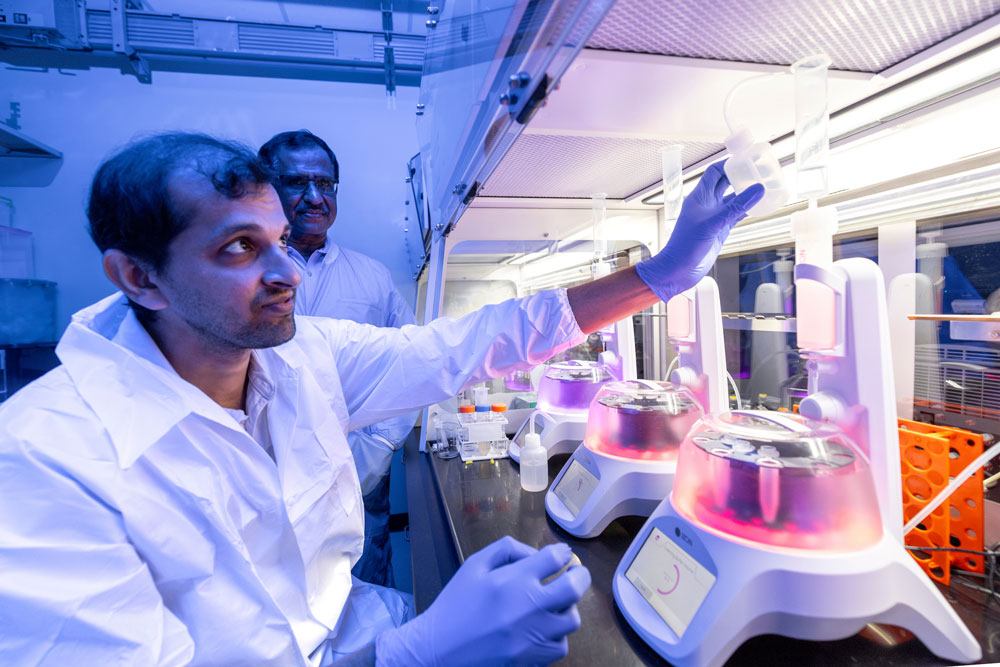
Shetty and his team have been working to develop what will eventually be a nasal spray that can be administered to patients with Alzheimer’s to improve their brain function, specifically by preserving cognitive and mood functions or slowing down the rate of cognitive decline. A vital benefit of this treatment is time — for patients, more time with their memories and independence, and for family and friends, more time with their loved ones.
“I’m a neuroscientist dedicated to developing new therapies,” Shetty said, “so my job and passion are to find a cure for difficult-to-treat neurodegenerative diseases such as dementia. So if I am successful, I’ll be extremely happy — not only for the patients with Alzheimer’s, but also the family members of patients with Alzheimer’s.”
A Closer Look at Alzheimer’s Progression
Alzheimer’s is currently a leading cause of death in people aged 65 and older. When a person’s brain is affected by Alzheimer’s disease, it develops an excess of a protein called amyloid beta, creating harmful plaques around the neural cells. In response to this, “housekeeping” cells called microglia are over-activated in an attempt to clean up the plaques, but this over-activation causes inflammation in the brain, sickening the neurons over a period of time.
In addition to these plaques and inflammation, within the neural cells, an abnormal form of a protein called tau begins to form, resulting in “tangles” in the neurons. The combination of the plaques outside the neurons, the tangles inside the neurons and the overall inflammatory environment causes the neurons to become sicker and sicker, losing vital connections (synapses) between each other and eventually dying.
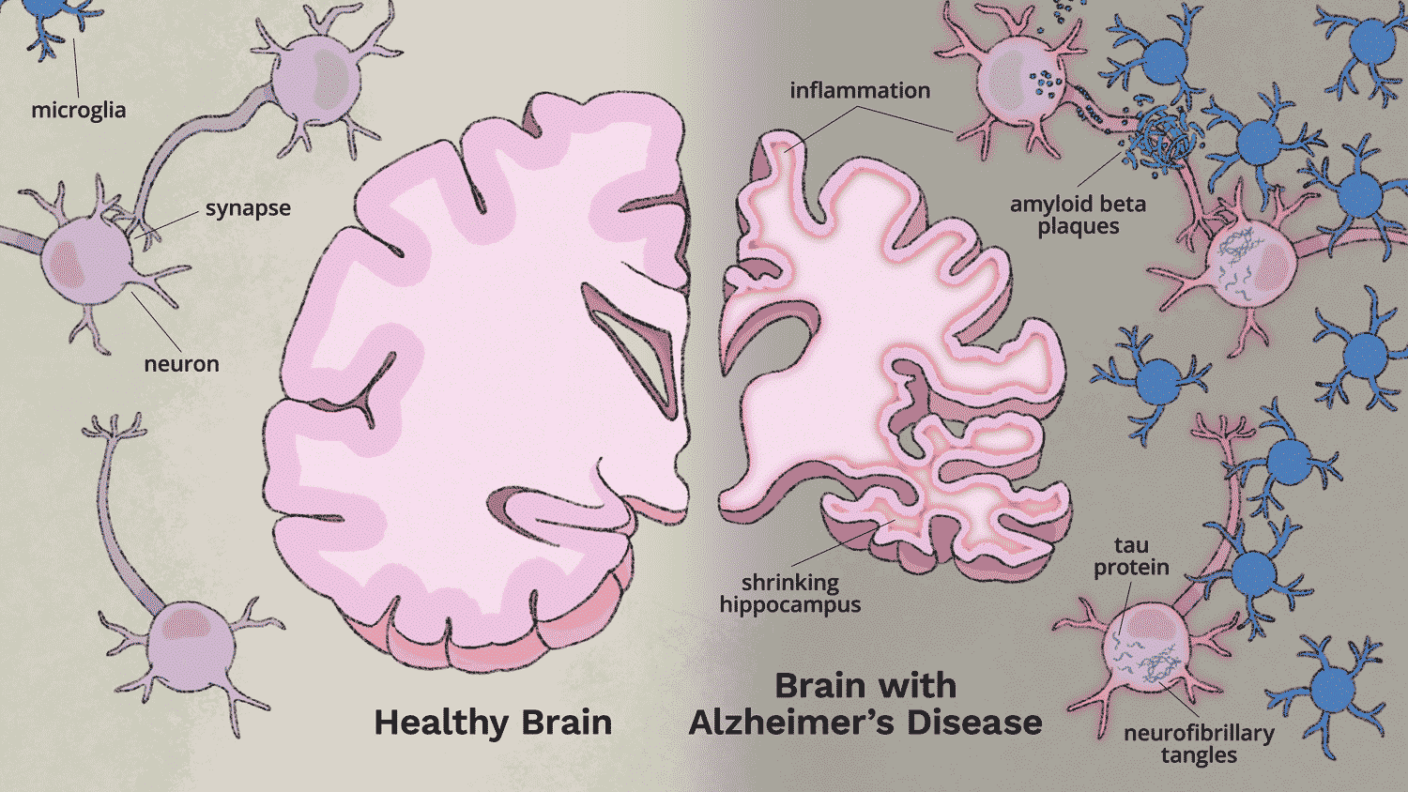
With loss of synapses — important for neural activity and memory formation — reduced numbers of neurons, and an adverse environment that cannot produce new neurons in the hippocampus, the brain’s learning and memory center, the person experiences a decline in memory and cognitive function. In the final stage of the disease, the brain undergoes massive neurodegeneration.
“In the later stages of the disease, what happens is the patients will stop recognizing family members, and then in the much more advanced stages, they don’t even know who they are. That leads to a lot of confusion, aggressive behavior and depression, so it’s very hard on the families.”
A Way to Stop the Spread
While there is still no cure for Alzheimer’s, the treatment being developed by Shetty and his team has shown great success in slowing its progression and even reversing some of the damage inflicted on the brain. The solution could mean years of improved brain function added to the lives of those with the disease.
The treatment begins with nanosized vesicles — tiny pockets of fluid — made out of human neural stem cells. The nasal mucous membrane must be permeated for the vesicles to quickly enter the entirety of the brain to be taken up by various types of brain cells. Once inside the brain, the vesicles work in a number of ways:
- Their cargo modifies the microglia to prevent them from overactivation while allowing them to function at a healthy level, cleaning up plaques. This, in turn, also decreases inflammation.
- They target the abnormal form of tau protein, reducing the number of tangles in the neurons.
- They protect neurons from the harmful effects of the amyloid-beta protein, including the buildup of plaques and tangles.
- They trigger the production of new neurons in the hippocampus, the brain’s learning and memory center.
Together, the result of these various vesicle functions is improved brain function and a reduction in the effects of Alzheimer’s. This translates into a higher quality of life and the priceless gift of time, especially if treatment begins in the early stages of the disease.
“Alzheimer’s disease is progressive,” Shetty explained. “After the diagnosis, it takes about an average of four to eight years to get into that advanced stage. But when we intervene very early with these extracellular vesicles, we could potentially delay the Alzheimer’s disease progression by up to 10 years. We are also testing whether periodic treatment with vesicles can preserve improved brain function for even longer periods.”





Photos by Abbey Santoro/Texas A&M University Division of Marketing & Communications
Having tested the treatment in the early stages of Alzheimer’s, the results have been overwhelmingly successful. Shetty has recently applied for a patent, the next step in making the treatment available to the public. However, the road is still long, with many steps along the way before clinical trials can begin.
“The first hurdle is making clinical-grade extracellular vesicles, which could receive FDA approval for a clinical trial in patients with Alzheimer’s,” he said. “So, we also need to collaborate with biotech companies because we need cGMP (Current Good Manufacturing Practice) facilities for that, and we need to develop protocols that are compliant with the FDA regulations for clinical trials.”
The vision for the final product of Shetty’s research is a noninvasive nasal spray that contains the vesicles and is available through a quick doctor’s office visit or even at pharmacies. This accessibility is possible through the scalability of the vesicles, which would also make the treatment more affordable for the public. The bold new approach could be a revolutionary leap from the current treatment options to an easily accessible, effective, self-administered spray, extending and improving the lives of countless individuals.
Heart Behind the Research
Shetty and Souza have always been interested in studying the mechanisms of brain aging, but Souza’s motivation to find neurological advancements escalated when her grandmother began battling dementia. Now, as a collaborator of Shetty’s research program, she knows from personal experience the impact this research could have.
She says that she has always been fascinated by how brains age differently, but her grandmother’s experience gave her a front-row view of how these differences deeply affect lives. Not only was it incredibly hard for her to watch the dementia progress in her grandmother, but she said she also felt very alone, and despite being part of a large Alzheimer’s research community, it was difficult to find the resources she needed to help her grandmother.
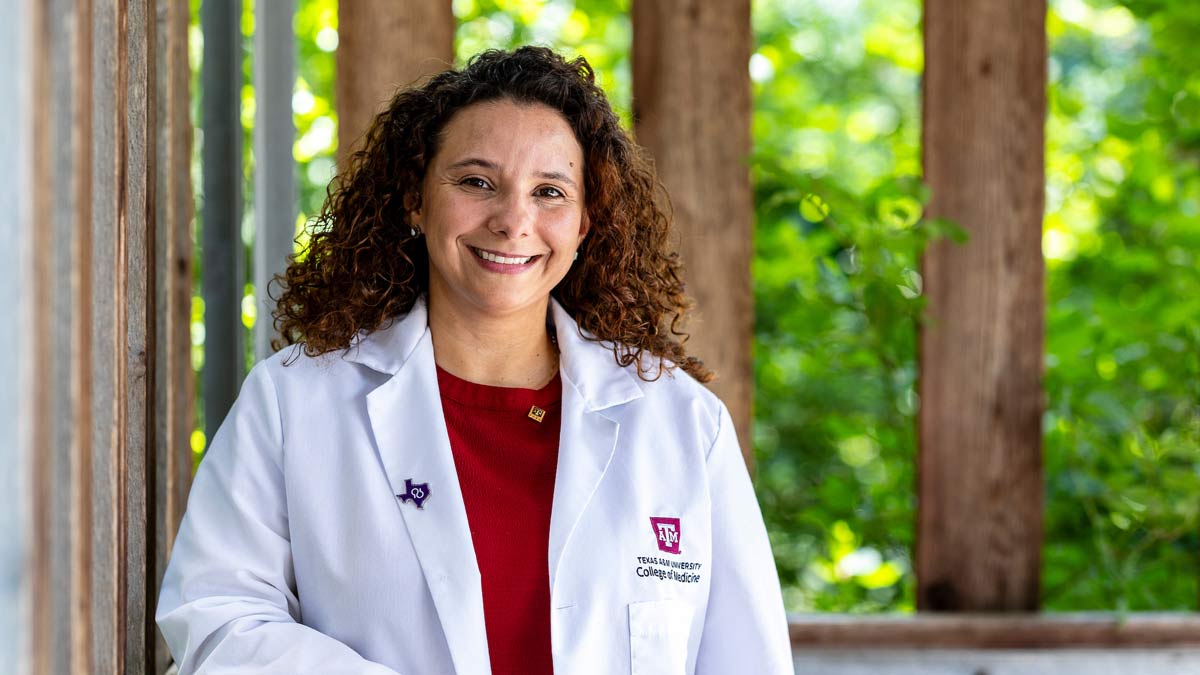
Going through the disease with my grandmother, it just ignited the need for me that we need to reach out to the community, that we need to explain what we’re doing in the lab so they know where we are in terms of coming up with a therapy and a cure.
“Going through the disease with my grandmother, it just ignited the need for me that we need to reach out to the community, that we need to explain what we’re doing in the lab so they know where we are in terms of coming up with a therapy and a cure. And I do believe that the community can understand what the treatment is and what it does. I think that bridge can be crossed.”
Especially now that Texas A&M researchers are close to a meaningful solution, it’s as important as ever to share the news with those who are currently suffering, whose loved ones are suffering or who might come face to face with a diagnosis later in their lives.
Souza is very optimistic about the new method Shetty has discovered to fight the disease. She said that he has gone “against the grain” of other Alzheimer’s research by being the first to try a new treatment method that targets inflammation in the brain. This has allowed a door to be opened to a revolutionary new remedy that could benefit millions around the world.
Both Shetty and Souza agree that this research exemplifies the core of what Texas A&M is all about — producing solutions that impact Texas, the nation and the world. Fueled by a deep desire to better understand one of the body’s most complicated organs, the goal for this project is to serve humanity by relieving millions of individuals and families from the pain brought by Alzheimer’s.

Shetty’s research team includes various scientists and students who share a goal of finding a way to slow and even reverse the progression of Alzheimer’s disease.
In recognition of the massive potential impact this solution has, the treatment recently garnered attention as a “World-Changing Idea” honoree by Fast Company magazine, a leading business media brand that focuses on innovation in a broad array of fields. In addition to honoring the awardees, the platform allows the selected researchers to get the word about their projects out to a very wide audience.
However, Shetty has never been motivated by recognition, but by his fascination with the brain and the potential of helping solve one of its most far-reaching complications — Alzheimer’s disease. And with the work he’s doing alongside his research team at Texas A&M, the solution may be closer than ever before.
