Building breath, layer by layer: 3D printing with living lung cells in extreme environments
Texas A&M researchers are studying how human airway cells respond to extreme pressure and heat — insights that could improve safety for pilots and astronauts while advancing drug discovery and respiratory disease research.
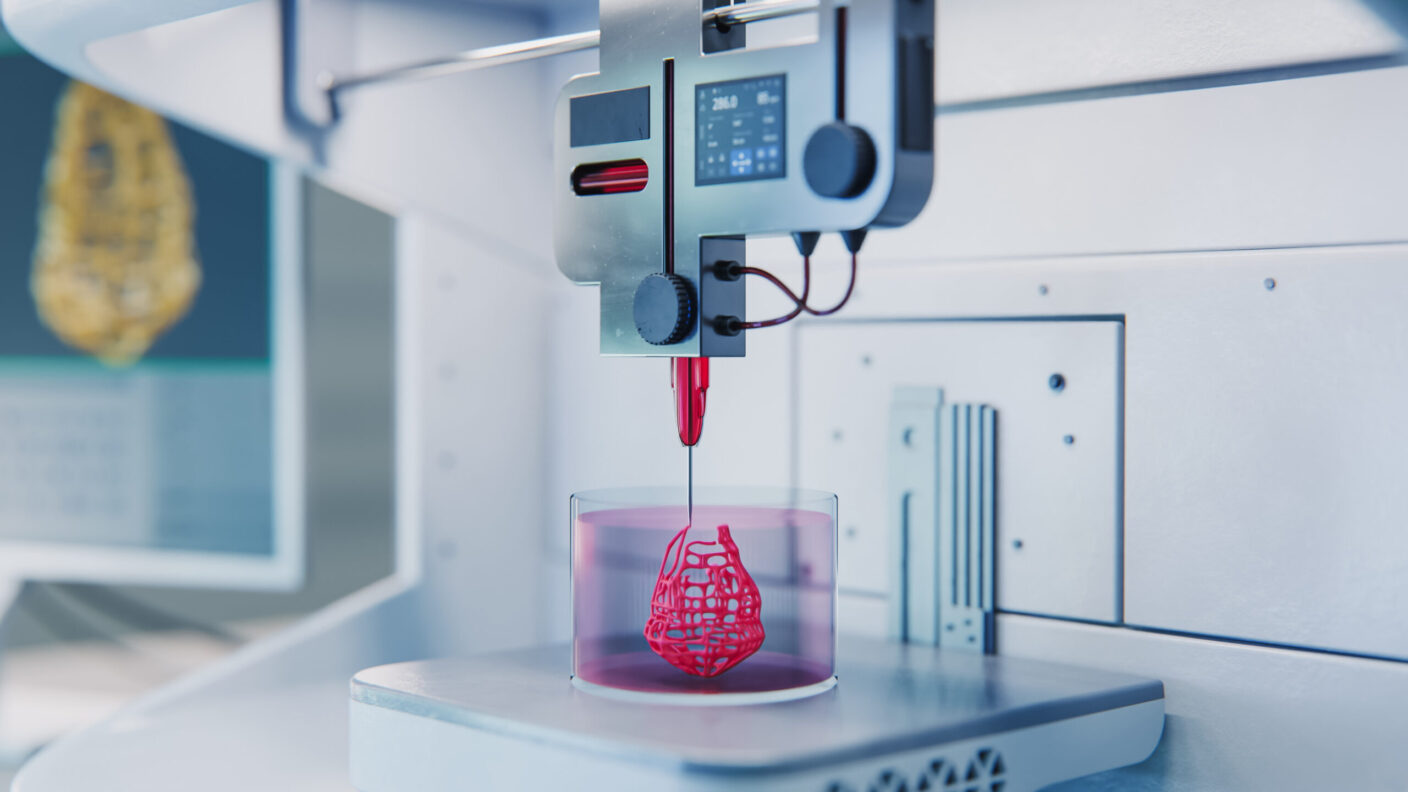
Researchers at Texas A&M University model extreme conditions using 3D bioprinting, revealing insights that could make flight and space travel protocols safer while driving new breakthroughs in respiratory disease research and drug discoveries.
When pilots take to the skies or astronauts venture into low orbit, their bodies face extreme conditions that traditional cell cultures can’t fully mimic.
Now, researchers at Texas A&M University have found a way to model these extreme conditions: using 3D bioprinting.
Led by College of Engineering professor Dr. Zhijian “ZJ” Pei in collaboration with College of Arts and Sciences professor Dr. Hongmin Qin — and supported by the U.S. Air Force Office of Scientific Research— the project could help improve safety in aviation and spaceflight, while accelerating how scientists study and treat respiratory diseases.
By investigating how 3D-bioprinted samples embedded with lung cells respond to physical stress, we’re advancing the fundamental principles of the effects of extreme environments on human biological systems.
Engineering the ideal airway model
The researchers’ approach is as precise as it is innovative.
Loading a gel-like bioink containing living cells into cartridges, the researchers carefully printed samples layer by layer.
Unlike traditional 2D cell cultures, their 3D approach offers a more realistic picture of how human cells behave under stress.
“With our 3D approach, we can closely mimic native tissue and their microenvironments, enabling accurate studies of viability, proliferation and stress responses,” Qin said.
It’s a powerful tool for understanding how human cells cope with real-world extremes.
Extreme conditions, like elevated temperatures, crushing pressures and limited oxygen, can have a serious toll on the human body — sometimes with life-threatening consequences.
For flight crews and space personnel, rapid changes in pressure or altitude can cause dangerous fluid buildup in the lungs, while high temperatures can trigger strokes, tissue damage or lead to organ failure.
“Our findings shed light on how lung cells respond to physiological and mechanical stressors, including variations in pressure and temperature,” Qin said. “Potential applications could enhance safety protocols for pilots and astronauts in low-orbit conditions.”
Beyond aerospace, the approach also offers a realistic model for studying respiratory diseases that pose major global health concerns, like chronic obstructive pulmonary disease, and potentially speeding up new drug discoveries.
In the long run, the researchers envision a process that could produce on-demand bioengineered tissues.

Our long-term goal is to develop engineered lung tissues in a controlled laboratory setting, providing a more realistic model for research than traditional 2D cell cultures.
Testing cells under extremes
The researchers’ approach highlights a key feat in bioprinting: balancing precise printing with cell survival.
“Even small adjustments in the bioprinting process can dramatically affect cell viability and proliferation,” Qin said. “By fine-tuning these parameters, we are laying the groundwork for future breakthroughs in tissue engineering.”
In one study published in Biomimetics, the team varied extrusion pressure during printing and found that higher pressures led to greater cell death.
Another study, published in Bioengineering, exposed the 3D-printed samples to elevated temperatures up to 55 degrees Celsius. The researchers observed that higher heat increased oxidative stress and reduced cell survival.
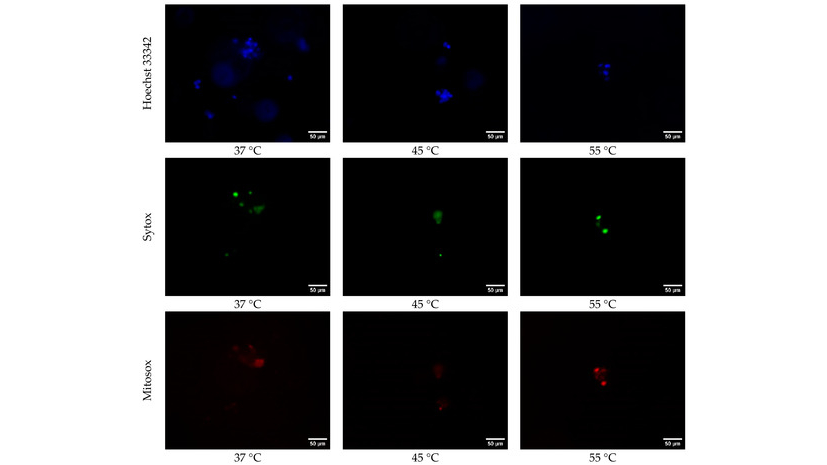
Heat takes a toll: fluorescence images reveal that as the 3D-bioprinted samples are exposed to higher temperatures, their stress levels rise and their survival is reduced.
“The pressure and temperature findings highlight the need for precise techniques to preserve the viability of lung cells in 3D-bioprinted samples, and demonstrate how the cells respond to environmental stressors,” Qin said.
The team also developed an optimized bioink — a 4:1 collagen-to-alginate mixture maintained an impressive 85% cell viability for six days.
“Defining the right bioprinting parameters allows us to replicate realistic conditions while preserving cell function,” Pei said.
Interdisciplinary innovation: The Texas A&M approach
At the heart of this U.S. Air Force-supported project is a powerful collaboration that exemplifies Texas A&M’s commitment of driving cutting-edge science into real-world impact — advancing both research and national defense priorities.
“We are bridging the gap between concept and applications that make a tangible difference,” Pei said.
For Pei and Qin, the 3D printing with lung cells is more than an achievement: it’s the foundation of innovation, the “ink” on which the next generation of technological breakthroughs is built — cell by cell, layer by layer.
